Clinical Ageing & Health: Frailty
- Camila Rahim

- Jul 6, 2020
- 6 min read
Updated: Jul 11, 2020
Today I will be discussing the Concept of Frailty with Musculoskeletal Conditions in Clinical Ageing & Health. I hope this post will deepen your understanding of frail elderly health and common diseases/disorders such as Osteoarthritis, Osteoporosis and Sarcopenia. If any of your family members or loved ones are facing this, do approach the doctor as it is potentially reversible and allows doctors to identify elderly with musculoskeletal conditions and address treatment intervention. Due to the increase in significant comorbidity and frailty in the ageing population, geriatricians and MDT (Multi-Disciplinary Team) need to take a holistic approach when assessing the elderly for better clinical practice and research design. MDT is a team of healthcare workers (eg. Occupational Therapist, Physiotherapist, Doctors, Nurses) in different disciplines working together to provide specific services to the patient.What is Frailty?
Frailty in later life is a common geriatric syndrome as it is associated with a loss of physiological reserves and function leading to an increase in vulnerability to poor health outcomes. This vulnerability compromised the elderly’s daily life such that minor stressors/illnesses may result in infection, disability, falls, organ failure, or death due to lack of resilience to recover. The concept of frailty in the Venn diagram figure below involves 3 very distinct entities (1) frailty: increased vulnerability to loss of function, (2) disability: loss of function, and (3) comorbidity: number of present diagnoses. It is important to understand that the concept of frailty only applies when a minimum of two concepts co-exist together for instance; ‘frailty’ and ‘disability’. In comparing two elderly; a healthy individual to an unhealthy frail individual and both suffered from a hip fracture, the healthier individual will recover well while the unhealthy frail individual will become more susceptible to stressors due to the loss of physiological reserves thus, worsen the disability and give rise to comorbidities as well.
In the ageing population, the prevalence of frailty increased exponentially with increasing age from 6.5% at age 60 – 65 years to 65% at ≥ 90 years in the UK. Similarly, more elderly are living with significant comorbidity. As all physiological functions decline with age, particularly the musculoskeletal system as it plays a major role as well as being closely linked to frailty. Frailty is associated with the common age-related musculoskeletal conditions: osteoporosis, osteoarthritis, sarcopenia, etc. Musculoskeletal system's primary functions are support, stability, and locomotion. Musculoskeletal functioning is the key component in determining frailty, as it leads to a loss of joint function, skeletal disorder, and reduced bone mass/density hence the musculoskeletal conditions. The pathophysiology of frailty enhanced the understanding of frailty in the ageing process and by focusing on the musculoskeletal system to promote a variety of treatment strategies for the medical professionals; eg. general practitioners to support the frail individuals.

Osteoporosis
Osteoporosis is a common bone disease and highly found amongst the elderly. Osteoporosis is characterized by reduced bone mineral density (BMD) due to micro-architectural deterioration of bone tissue that leads to an increased risk of fracture. Fractures will then cause significant morbidity and mortality, hence it is a major public health problem. The pathogenesis is the defect in attaining peak bone mass and/or accelerated bone loss with age; impaired osteoclasts (bone resorption) function that affected osteoblasts new bone formation process. However, the pathogenesis in the elderly differs by an increase in bone turnover and a decline in bone marrow ability to differentiate and form into adipocytes instead of osteoblasts (bone formation). Age is the main risk factor and oestrogen deficiency in postmenopausal women has a higher risk of osteoporosis-related fractures than men and the risk tripled at the age of 70 years due to accelerated bone loss. Other risks factors include falls, recurrent fractures, genetic, epigenetic, environmental, diet and lifestyle. In short, an elderly individual with low BMD in any bones will reduce bone strength, increase fragility fractures, and causing functional decline (disability) which characterizes frailty.
Osteoarthritis
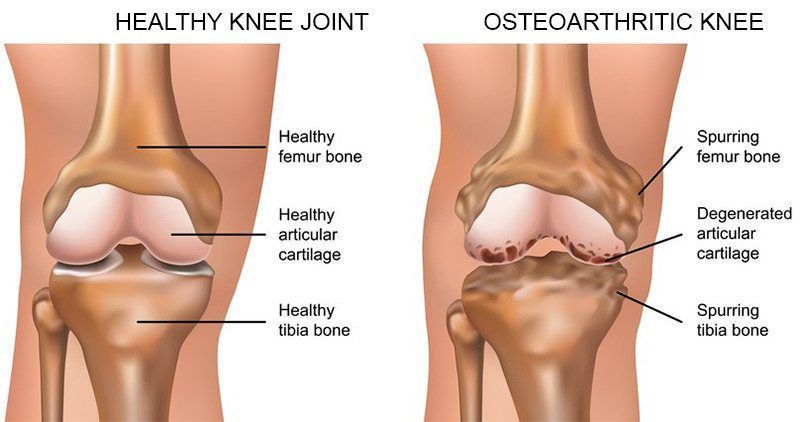
Osteoarthritis (OA) is the most common joint disorder and principally affects the ageing population. OA is characterized by loss of articular cartilage, osteophytes formation, subchondral osteosclerosis, low-grade inflammation which results in an increased risk of falls, pain, and disability. This progressive joint disorder rises to 10 – 15% of elderly age over 60 years and higher prevalence among women than men. The key pathophysiological mechanisms in ageing are pro-inflammatory (interleukins IL-6, IL-8), tumour necrosis factor-a (TNF-a), C-reactive protein (CRP) and pro-catabolic mediators. Common risk factors that contribute to the development of OA are age, genetics, obesity, lifestyle and joint trauma. In ageing OA, the joint structure integrity and function is already compromised by the loss of cartilage and mechanical load, thus an increase in pro-inflammatory processes and CRP will significantly worsen the joint condition and result to the onset of pain and disability.
A previous study by O’Brien and McDougall (2019), supported by Giovannini et al (2011), demonstrated a relationship between OA, age and frailty with ‘inflamm-ageing’; that refers to low-grade inflammation from pro-inflammatory markers during physiological ageing. Approximately 24% – 60% of OA individuals were significantly associated with frailty. Overall, it is known that OA causes pain, stiffness and weakness to the individual at large joints of the body and this severely impairs the activities of daily living (ADL) in the frail elderly. Despite research over the years, the pathogenesis of OA with ageing remains unclear and this negatively impacts the OA individuals and the drug development process for treatments. Since OA shares many similarities with frailty, and some studies suggested that sarcopenia contributes to the development of OA and frailty thus, sarcopenia might be closely associated with frailty.
Sarcopenia
Sarcopenia is an ageing syndrome and is the key component in the concept of frailty syndrome. Sarcopenia is characterised as a muscle disease by progressive loss of skeletal muscle mass and strength leading to disability, falls, fragility fractures, dependency and death. Risk factors include age, gender, diet (nutrition), lifestyle, physical activity and chronic diseases (obesity). Sarcopenia is caused due to disruption between the cell growth and cell break down of the skeletal muscle mass as we age. The pathogenesis remains unclear due to multiple causes and proposed pathways such as ‘inflamm-ageing’ has been suggested as a potential relationship between sarcopenia, OA and frailty. In contrast, there have not been any prospective studies directly linking ‘inflamm-ageing’ with the development of sarcopenia, OA and frailty. However, sarcopenia is multi-factorial (primary and/or secondary condition) and rapidly increases from the age of 50 years. Primary condition refers to age-related sarcopenia while secondary sarcopenia conditions could be activity-related, disease-related, nutrition-related and more. The European Working Group on Sarcopenia in Older People (EWGSOP) categorized sarcopenia based on the severity level; pre-sarcopenia, sarcopenia and severe sarcopenia by the number of criteria present; (1) muscle mass, (2) muscle strength and (3) physical performance. Severe sarcopenia (3 criteria present) could overlap with the concept of frailty, in particular, the muscle strength and low physical performance supported by Wilson et al (2017). As frail individuals with sarcopenia express significant physical disability that characterizes the concept of frailty, this supports sarcopenia as the key component to frailty syndrome. That said, there is still a need to increase public health awareness regarding sarcopenia to achieve a clearer definition and diagnostic criteria.
GP Intervention
The role of a general practitioner (GP) in geriatric is to prevent frailty by identifying early signs of frailty in the elderly by working with the MDT (Multi-Disciplinary Team) to perform CGA (comprehensive geriatric assessment). GPs are known as ‘gatekeepers’: the front line in primary care, their responsibility is to adequately screen the elderly who present with suspicious (present/past) falls, fractures, in order to identify and support those at risk of frail. MDT involves a team skill’s set from professionals; physiotherapists, occupational therapists, social worker to achieve good person-centred care for patients. Importantly, history taking is essential to build rapport and gather patient details, hence a thorough CGA, and frailty assessment; Rockwood score (figure shown below), Fried Frailty score, etc. CGA is fundamental in geriatric medicine, it quantifies frailty into 5 different aspects; (1) physical health, (2) mental health, (3) social aspects, (4) functional aspects, (5) environment. The information from CGA will then help in understanding the frailty assessment approach and relationship with frailty. Rockwood score is a common frailty assessment score-based approach to evaluate clinical frailty level shown below. Establishing a patient’s clinical frailty level supports decisions for further investigation, management, personalized treatment, social support, and any need for rehabilitation. A common treatment plan is an exercise programme, nutritional therapy, resistance training and smoking cessation. Mutualistic decisions between the patient and GP is one of the UK NHS Constitution values; ‘working together for patients’ which every GPs, professionals and healthcare worker are aware of. Thus, this is important for musculoskeletal health as approximately 70% of frailty assessments involves physical activity or mobility test. In summary, GP’s role is to take a holistic approach, prevent frailty and maintain good person-centred care by working closely with MDT and patients.

Hope you find this post useful!
Do read my other post regarding the financial support from the Singapore Government for the elderly or individuals with disabilities.
Follow me on my LinkedIn & Instagram: camilarahim






Comments